Part III-C: The Extraction Code Across Sectors
Benefits, Public Contracts, and Why the Pattern Survives Exposure
Series: The Extraction Code
Part I | Part II | Part III-A | Part III–B | Part III–C | Part IV-A | Part IV–B | Part V
Become an Investigative Partner. Paid members receive:
Daily Intelligence Briefings - Yesterday’s news, decoded by morning. See the extraction pattern before your second cup of coffee.
Weekly Case Files - One real victim. One institutional lie. Line-by-line deconstruction with courtroom-grade sources.
Monthly Pattern Reports - Connect the dots across healthcare, finance, and policy—the 30,000-foot view.
A framework you can apply in real time: who must enter, where friction is added, who can say no, and where gain concentrates.
Subscribe Now: Introductory offer: 25% off monthly and annual paid subscriptions through Jan 23, 2026.Benefits & Eligibility: The Bureaucratic Maze
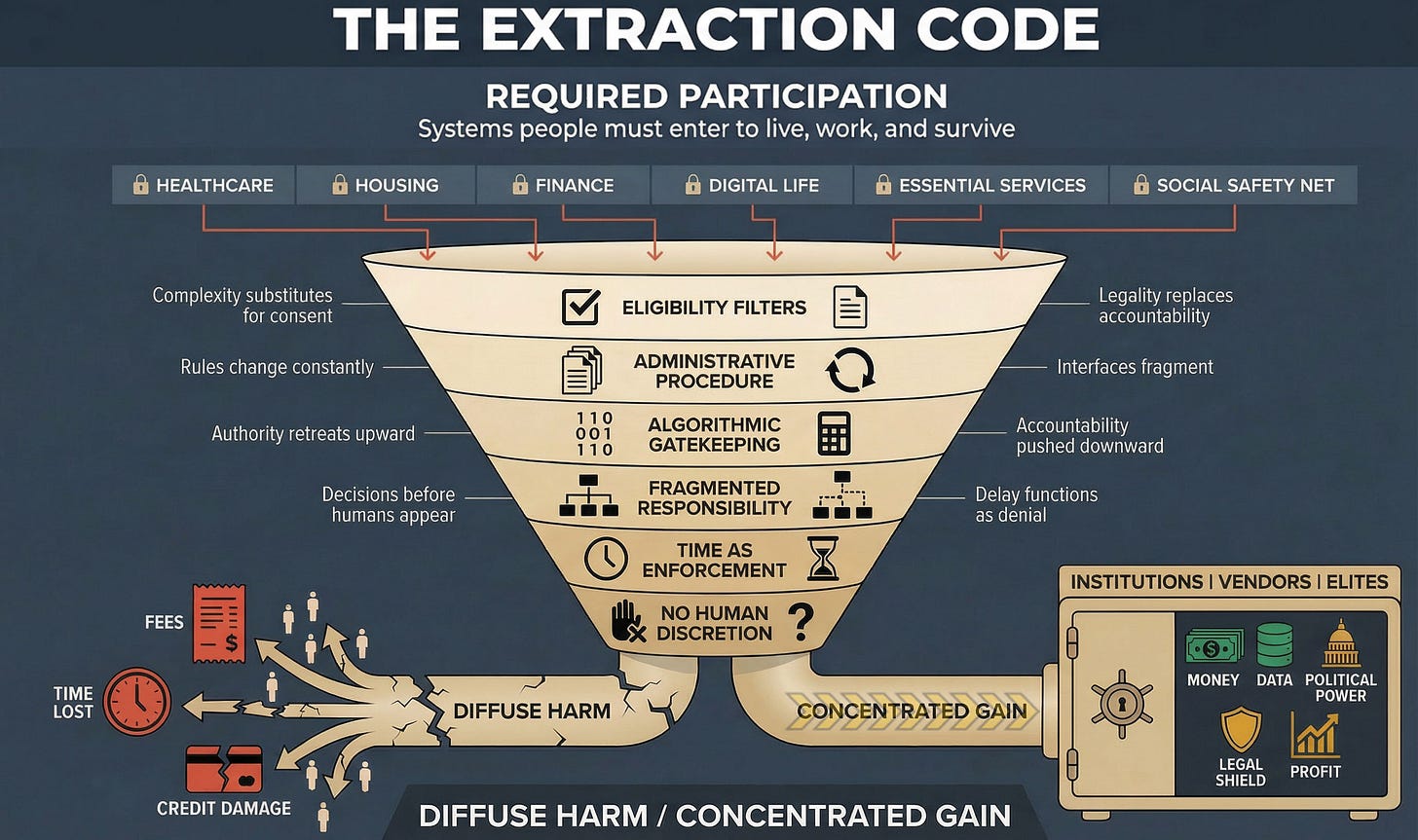
Required Participation
You cannot opt out of government benefits systems if you need them to survive. Medicaid, SNAP (food stamps), TANF (cash assistance), unemployment insurance, disability benefits, and housing vouchers are not optional services. They are a survival infrastructure for people; the market economy has failed.
And they are designed to be nearly impossible to access.
The Funnel in Action
Layer 1 - Eligibility Filters: Means-testing requirements that demand extensive documentation: pay stubs, tax returns, bank statements, asset verification, household composition details, citizenship or immigration status, work history, disability documentation, rental agreements, utility bills. Requirements change between the application and recertification. States have different rules. Counties have various interpretations. And you’re responsible for knowing all of it.
Example: You apply for Medicaid in a state that expanded under the ACA. The application requires: (1) proof of income for everyone in the household, (2) proof of residency, (3) Social Security numbers, (4) citizenship documentation, (5) asset verification (bank statements for the past 3 months), and (6) verification of any other insurance coverage. You’re working two part-time jobs with irregular schedules. One employer pays cash. The other uses a payroll app. You’re staying with family temporarily (you’re not on the lease). You don’t have a bank account (you cash checks at a check-cashing service).
You cannot provide half of what they’re asking for. And if you can’t prove eligibility, you’re denied, even though you’re clearly below the income threshold and desperately need coverage.
Layer 2 - Administrative Procedure: Applications must be submitted through state portals that crash, require specific browsers, don’t save progress, and time out after 15 minutes of inactivity. Documentation must be uploaded in particular formats (PDF only, under 2MB, scanned at a specific resolution). Deadlines are strict. Extensions are rare. Reapplications require starting over from scratch.
Example: Your state requires annual Medicaid recertification. You receive a notice in the mail: you have 10 days to submit updated documentation or your coverage will be terminated. The notice arrived 7 days ago (mail delay). You have 3 days to gather the pay stubs, upload them to the portal, and submit them. You try to log in, but the portal is down for maintenance. You call the helpline, with a 3-hour wait time. You finally reach someone, and they cannot accept documentation by phone or email; you must use the portal. The portal comes back online 2 days later. You upload documents. Error message: “File format not supported.” You convert to PDF. Upload again. Error: “File size too large.” You compress the PDF. Upload again. Success. You check the next day, case status shows “pending.” You check again in a week, and the coverage will be terminated for “failure to provide documentation.” You submitted it on day 9. They say they didn’t receive it until day 12. You’re uninsured. Your child’s medication costs $400/month. You cannot afford it. You appeal. The appeal takes 30 days. Your child goes without medication.
Layer 3 - Algorithmic Gatekeeping: Many states now use algorithmic eligibility determination systems that automatically deny applications based on data matching, fraud detection algorithms, and predictive models that claim to identify “high-risk” applicants.
Example: You apply for SNAP benefits. The system cross-references your application against: (1) employment databases, (2) wage records, (3) DMV records, (4) utility payment histories, (5) address verification databases, and (6) fraud detection algorithms that flag “suspicious patterns.” You’re flagged because your address doesn’t match utility records (you’re staying with family) and your employment history shows gaps (you were caregiving for a parent). Your bank account shows irregular deposits (you do gig work). The algorithm determines you’re “high risk” for fraud. Auto-denied. You never spoke to a human. The decision was made by pattern-matching software designed to minimize program costs, not to feed hungry people.
Layer 4 - Fragmented Responsibility: Who denied your benefits? The state agency? The eligibility contractor they hired (Maximus, Conduent, Accenture)? The verification vendor (LexisNexis, Equifax Workforce Solutions)? The fraud detection algorithm (built by a private tech company)? The answer is deliberately unclear. When you call, the state says they’re just following the contractor’s determination. The contractor says they’re just implementing the algorithm. The algorithm’s vendor says they’re just analyzing data. The data comes from third-party databases you’ve never heard of, aggregating information you never consented to share.
Layer 5 - Time as Enforcement: Application processing takes 30-90 days. Recertification is annual, but if you miss the deadline, you’re terminated immediately and must reapply from scratch. Appeals take 60-90 days. During that time, you’re without benefits. If you need food assistance now, if your child needs healthcare now, if you’re about to be evicted now, the system has no mechanism for urgency.
The timeline is designed to maximize attrition. People who cannot survive 90 days without assistance will give up, find other means (often harmful: payday loans, skipped medications, food insecurity), or fall through the cracks. The system counts on this. Fewer people receiving benefits = lower program costs = political success.
Layer 6 - No Human Discretion: When you call to ask why you were denied, you reach a call center worker who cannot see the algorithm’s decision logic, cannot override the determination, cannot grant exceptions, and cannot escalate beyond filing an appeal, which goes back into the same automated system that denied you in the first place. There is no caseworker with authority to look at your situation and say, “This person clearly qualifies, let’s approve them.” That discretion has been deliberately eliminated and replaced with algorithmic processing designed to say “no” as often as legally permissible.
The Output
Diffuse Harm: People who qualify for assistance but cannot navigate the process go without food, healthcare, and housing support. Children suffer from malnutrition. Families become homeless. People with disabilities lose SSI because they couldn’t complete the recertification paperwork. Elderly people lose Medicaid because they didn’t understand the new portal requirements. Immigrants avoid applying altogether because they fear data-sharing with ICE.
Concentrated Gain: Contractors billing the government to administer these programs profit from complexity, more verification steps = more billable processes. Technology vendors license their eligibility algorithms across multiple states. Fraud detection companies profit from flagging applicants (paid per flag, regardless of accuracy). And politicians claim credit for “reducing fraud and waste” when they’ve actually just made it harder for eligible people to receive help.
Paid subscribers get the exact counter-move checklist you can use today:
📊 Daily: 3 extraction signals with immediate counter-moves
🔍 Weekly: Investigative Case Files (decoder tables, accountability maps)
📈 Monthly: Sector Pattern Reports (what is brewing before it breaks)
The Pattern Across All Sectors
Look at what repeats:
Required participation you cannot opt out of → Eligibility filters that impose complexity as gatekeeping → Administrative procedures that fragment interfaces and shift costs onto individuals → Algorithmic decisions that eliminate human judgment and operate in proprietary secrecy → Fragmented responsibility that dissolves accountability across vendors and contractors → Time delays that function as denial by attrition → Elimination of human discretion that makes appeals futile and exceptions impossible.
Every sector. Same funnel. Same outcome.
This is not a coincidence. This is not bureaucratic incompetence. This is not “the system overwhelmed by demand.”
This is design.
The same consulting firms (McKinsey, Deloitte, Accenture) sell “efficiency optimization” to hospitals, insurers, government agencies, and platforms. That optimization always means the same thing: automate decisions, fragment accountability, eliminate discretion, impose friction, maximize extraction.
The same technology vendors (Palantir, LexisNexis, FICO, CoreLogic) sell algorithmic gatekeeping systems across sectors, repackaging the same risk-scoring, fraud-detection, and eligibility-filtering tools, whether the customer is an insurer, landlord, lender, or benefits agency.
The same legal strategies (mandatory arbitration, proprietary secrecy, terms of service, contractual immunity) get copied from tech platforms to healthcare systems to government contractors, because they work. They insulate extraction from accountability.
Why This Matters
Once you see the pattern, you start to have a chance.
The insurance claim that requires three appeals, the housing application that demands 15 documents, the credit report error that takes 90 days to dispute, the platform suspension with no human review, and the benefits recertification that terminates coverage for missing a deadline you never received; they are all the same system.
Different sectors. Different language. Same infrastructure.
And that infrastructure was deliberately built, continuously refined, and legally defended by people who profit from making access difficult, accountability impossible, and resistance futile.
Exposure does not stop this machine.
Understanding the design is the first step toward dismantling it.
Next in this series: Part IV will examine Michael Cohen’s testimony as the decoder key, how his 2019 congressional hearing revealed the linguistic and operational patterns that allow extraction to operate “in code,” maintaining plausible deniability while causing systemic harm at scale.
Barking Justice Media LLC publishes the Extraction Code Monthly Pattern Recognition Report. This report is part of our paid subscriber tier.
The Extraction Code” is an analytical framework developed by Mika Douglas.
The name, definitions, terminology, and structured mechanisms associated with The Extraction Code constitute original authored work.
Commercial use, derivative frameworks, training programs, or branded applications based on this work require prior written permission.


This breakdown of the Medicaid eligibility maze is painfuly accurate. The point about algorithmic gatekeeping eliminating human discretion hits hard - I've seen cases where folks who clearly qualify get auto-denied becuase of data mismatches they can't even access or challenge. The "time as enforcement" layer is especially insidious, using 90-day waits as a form of administratve denial knowing people cant survive that long without benefits.